At LGTC Group, we frequently encounter a specific type of client: intelligent, resilient, and successful, yet profoundly exhausted by a silent, internal battle. They have often reached the end of the road with traditional treatments, having cycled through talk therapy and standard medications with little lasting relief. If this describes your experience, it is vital to internalize a crucial truth: continued suffering is not a failure of character. It is very likely a limitation of the tools available to you until now.
For over half a century, psychiatry has relied on a single model of treating mood disorders. While helpful for many, it has left a significant portion of the population trapped in treatment resistance. Today, neuroscience offers a genuine paradigm shift. Ketamine-Assisted Psychotherapy is distinct because it works fundamentally differently. It does not simply adjust the volume on existing brain signals; it addresses the neurobiology of mental illness at a structural level. It is less about chemical management and more about architectural repair.
To understand why this offers scientifically grounded hope, we must look at the actual infrastructure of the healing brain. This article will break down the complex neuroscience of Ketamine, explaining why it is considered the most significant development in psychiatry in decades.
1. The Limitations of the “Serotonin Model”
To appreciate why Ketamine is revolutionary, we must understand why traditional approaches often fail complex cases. For over 30 years, care has centered on the “monoamine hypothesis”—the idea that depression and anxiety are caused by a simple deficiency of neurotransmitters like serotonin, norepinephrine, and dopamine. Consequently, the standard treatments have been Selective Serotonin Reuptake Inhibitors (SSRIs), which work by increasing the available amount of serotonin in the synaptic gap between neurons. The theory is that more serotonin equals better mood.
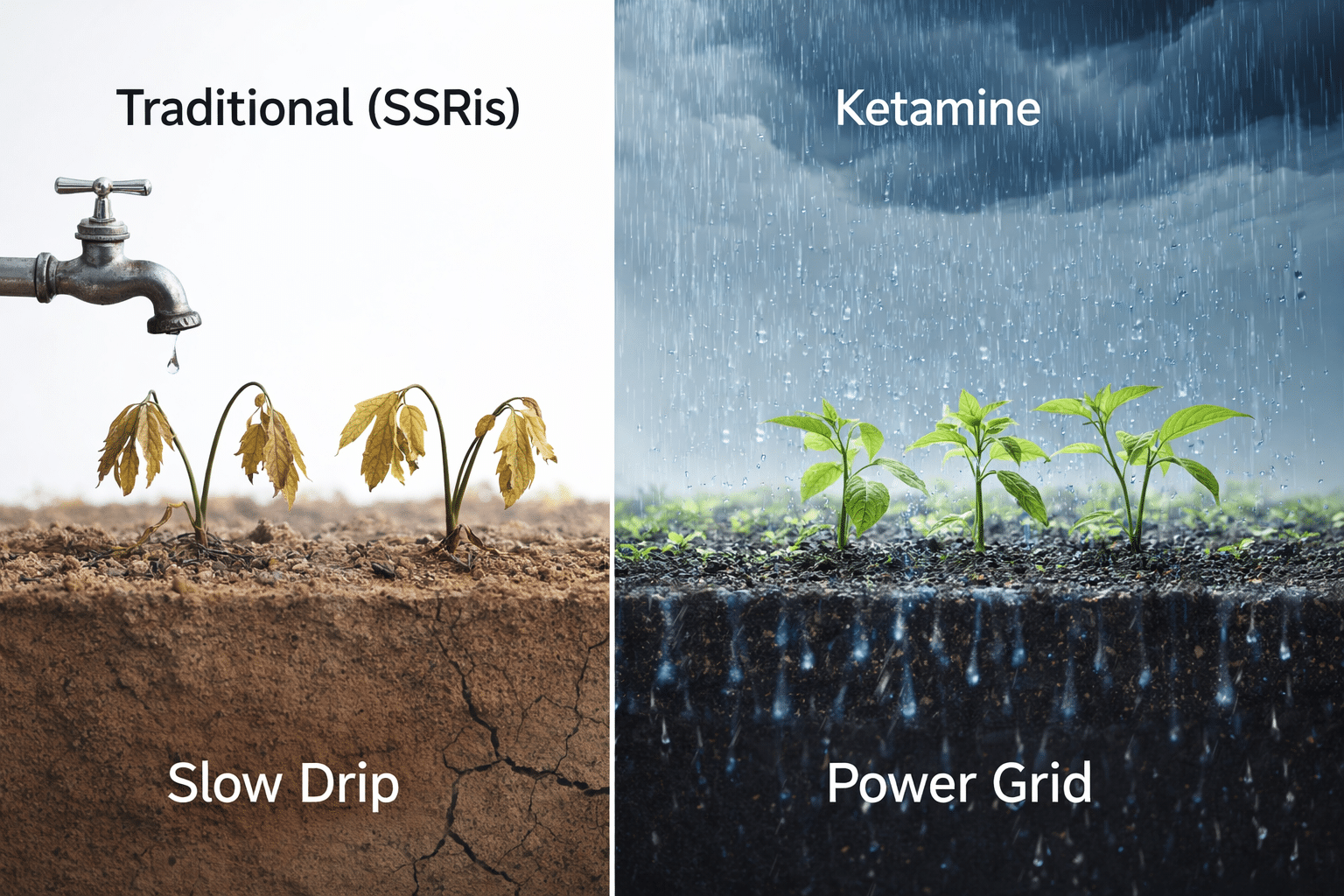
The “Slow Drip” Analogy
Think of a depressed brain like a vast garden suffering from a prolonged drought. SSRIs are akin to watering that garden with a slightly leaky faucet. Over months, the slow drip might accumulate enough moisture to help some plants survive. It provides a baseline, but it lacks the power to rapidly revitalize a parched landscape that has begun to wither.
Furthermore, clinical reality often conflicts with the theory. While SSRIs increase serotonin almost immediately, patients typically don’t feel relief for four to six weeks. This suggests serotonin is only part of a slower downstream process. For roughly 30% to 50% of patients with major depression—and more with complex trauma—this model simply does not work well enough. Their brains have adapted, and simply adding more of a single neurotransmitter is insufficient to break the cycle of rigid, negative thinking. We needed a way to move beyond the leaky faucet and access the brain’s main power grid.
2. The Paradigm Shift: Enter Glutamate
Modern neuroscience has moved away from viewing mental health disorders solely as “chemical imbalances.” We now understand disorders like chronic stress, trauma, and Treatment-Resistant Depression (TRD) as disorders of synaptic connectivity. Prolonged exposure to stress hormones like cortisol acts as a toxin, causing the critical connections between neurons—synapses—to wither and disconnect, particularly in areas responsible for emotional regulation and memory. The depressed brain essentially disconnects from itself, leading to cognitive fog and emotional numbness.
To repair this, we must look beyond serotonin to Glutamate. While serotonin influences mood, it is a minority neurotransmitter. Glutamate, conversely, is the brain’s primary “excitatory” neurotransmitter, accounting for over 90% of synaptic activity. It governs learning, memory, and neuroplasticity. If serotonin is the background music in a restaurant, glutamate is the conversations happening at every table combined.
In a depressed brain, the glutamate system becomes dysregulated—either underactive or chronically overactive, leading to cellular exhaustion. Traditional antidepressants barely touch this system. Ketamine’s brilliance lies in its ability to interact directly and rapidly with this massive glutamate power grid.
3. The Mechanism: The NMDA Receptor and the Surge
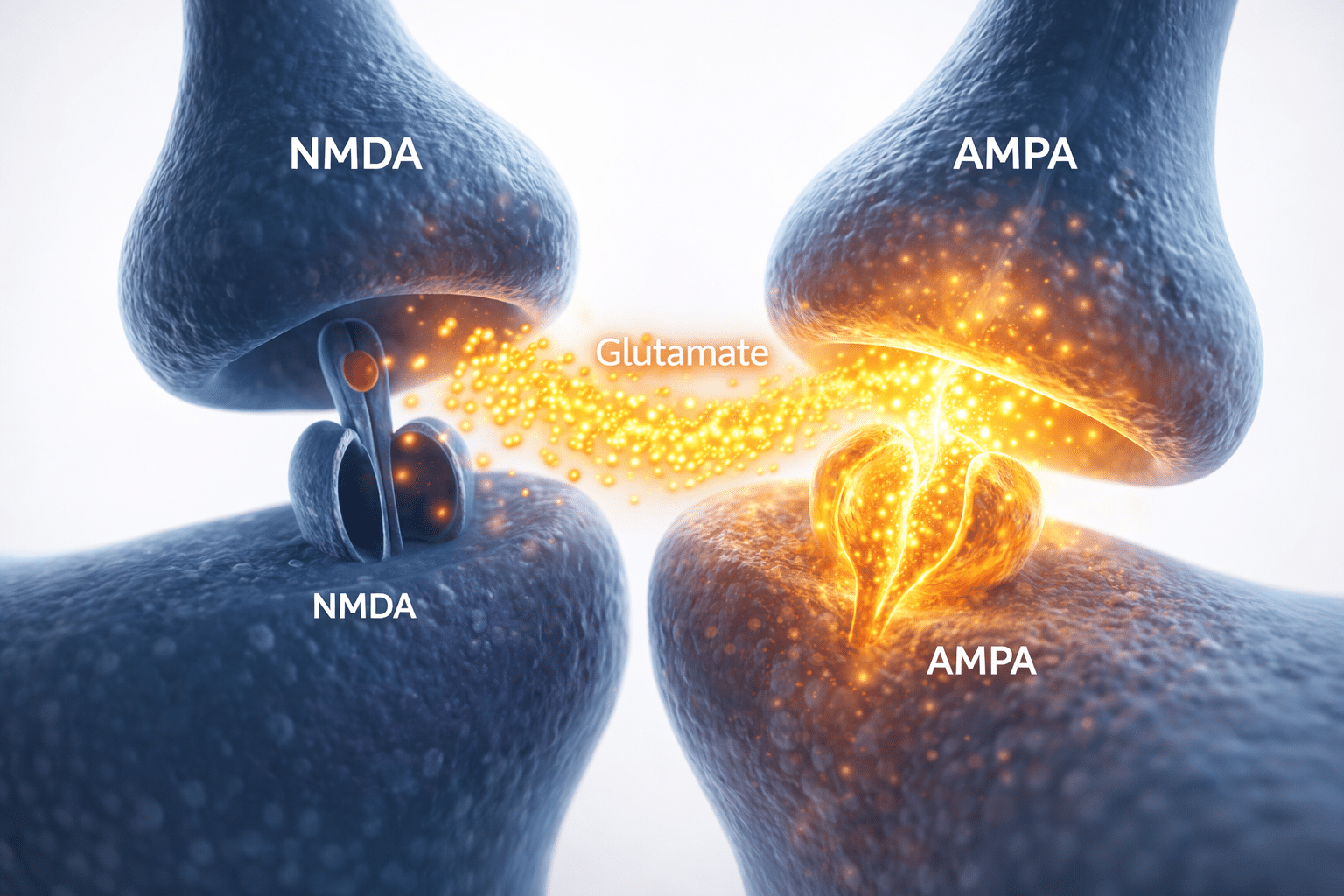
How does Ketamine repair a disconnected brain? The mechanism is fascinating. To speed up connectivity, Ketamine first has to block a specific door. It operates as an NMDA receptor antagonist. The NMDA receptor is a complex gate on a neuron designed to receive glutamate messages. Under chronic stress, the delicate balance of these receptors is thrown off; some become overactive, contributing to “noise,” while healthy pathways atrophy.
When administered in a controlled clinical setting, Ketamine molecules temporarily block these NMDA receptors.
The “Traffic Jam” Effect
Imagine a congested twelve-lane highway where the primary off-ramp is blocked. The traffic—glutamate—doesn’t disappear; it surges toward other available routes. By blocking the NMDA receptor, Ketamine forces a rapid surge of glutamate activation toward AMPA receptors, which are responsible for fast, immediate electrical signaling.
This sudden surge acts as a massive wake-up call to dormant parts of the brain. It is an immediate interruption of the depressed status quo. This explains why many patients feel a profound shift in perspective or a lifting of heaviness within hours, rather than weeks. But this immediate relief is only the catalyst for the healing that follows.
4. The Miracle-Gro Effect: BDNF and Synaptogenesis
The initial glutamate surge sets off a crucial biochemical cascade that continues long after the medicine has left your system. The most important result is the accelerated production of Brain-Derived Neurotrophic Factor (BDNF).
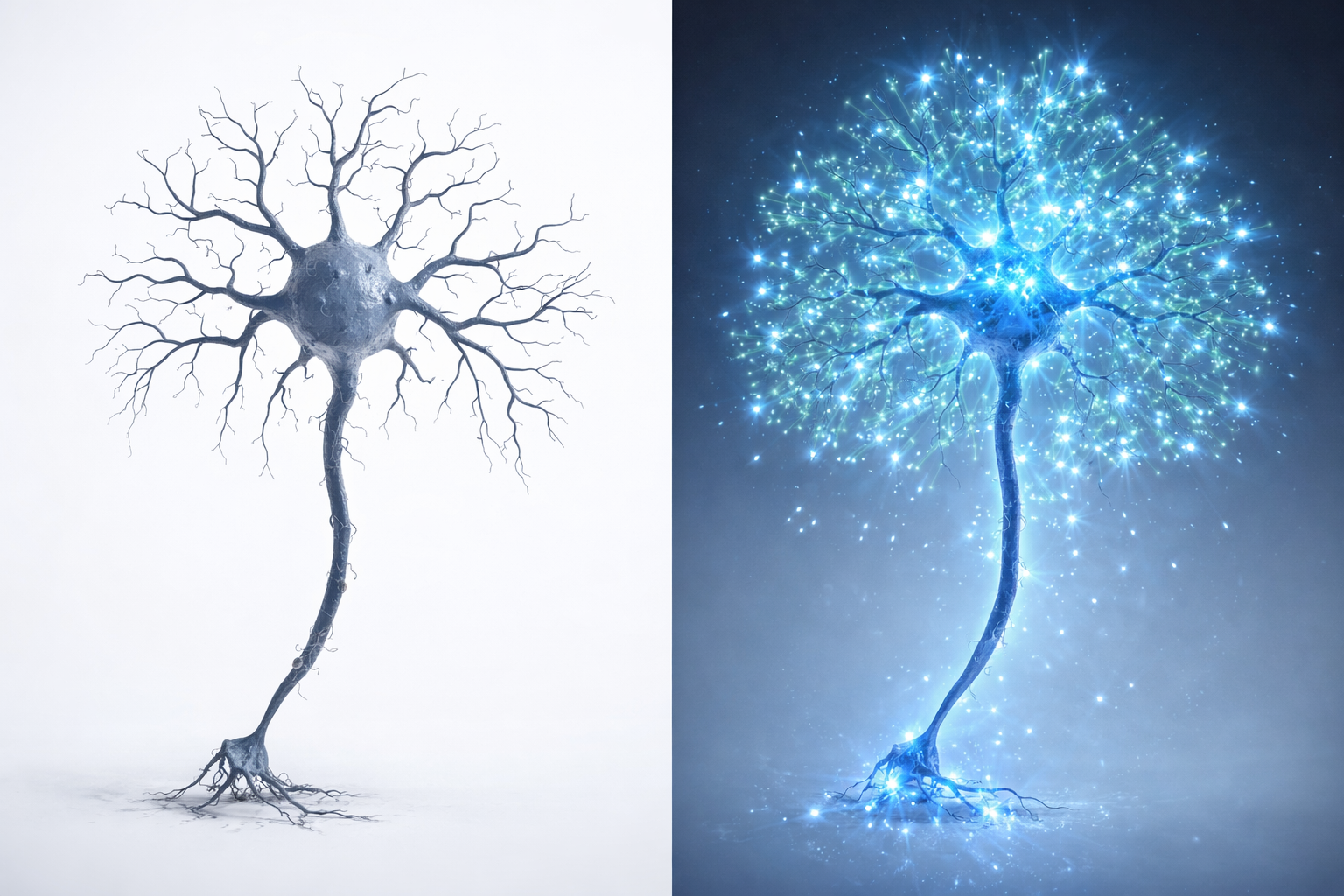
Nicknamed “Miracle-Gro for the brain,” BDNF is a powerful growth factor that supports neuron survival and encourages the growth of new synapses. As mentioned, a brain suffering from depression is physically different; stress causes dendrites to shrivel like tree branches during a drought. This physical retraction means the neural hardware necessary for resilience and joy is literally disconnected. This is why telling someone to “just think positively” is often futile; they lack the infrastructure to process that thought.
BDNF is the antidote. When Ketamine triggers BDNF release, it immediately begins to repair damage. This process, called synaptogenesis, allows researchers to observe damaged neurons sprouting lush new dendritic spines within 24 hours, physically rebuilding the brain’s communication infrastructure.
5. The Ultimate Goal: Neuroplasticity and Rewiring
The combination of the glutamate interruption and the BDNF-fueled regrowth leads to the ultimate goal: Neuroplasticity. This is the brain’s ability to change and reorganize itself, and it is the biological basis of hope.
When someone suffers from TRD or PTSD, their brain often gets stuck in rigid, negative feedback loops—deep ruts worn into a dirt road over years of travel. The more you think self-critical thoughts, the deeper the ruts get, and the harder it is to steer out. Standard therapy often feels like trying to steer out of these ruts while moving at full speed.
Ketamine addresses these ruts in two ways:
- The Fresh Snow (The Interruption): The glutamate interruption acts like fresh snow falling over those deep ruts. Suddenly, the old, negative paths aren’t so automatic. You have a critical window of objectivity where you are not ruled by reactive patterns. A crippling thought might suddenly feel distant or irrelevant.
- The New Road Construction (The Regrowth): The BDNF release provides the materials to build entirely new roads.
The Crucial Role of Therapy
This is why LGTC Group emphasizes Ketamine-Assisted Psychotherapy. Ketamine opens a “window of opportunity” for neuroplasticity lasting several days where the brain is uniquely malleable. Whatever you do during this window is amplified. If you return to a stressful environment, you might deepen negative pathways. However, when integrated psychotherapy is applied during this window, it is profoundly effective. Our therapists use this time to help you forge new neural pathways and practice new behavioral responses. We aren’t just patching holes; we are helping you redesign the roadmap of your mind.

Conclusion: Clinical Excellence in a Sanctuary Setting
The neuroscience of Ketamine is compelling. It offers a sophisticated mechanism for rapid recovery where standard treatments have failed, changing the conversation from symptom management to architectural repair. However, Ketamine is a powerful tool that requires sophisticated handling. The biological shift it initiates can be intense, and the setting is as important as the molecule itself.
At LGTC Group, we provide more than medical administration. We provide a bespoke sanctuary where this neurological resetting can occur safely under the guidance of world-class psychiatrists. We understand the exhaustion of treatment resistance. By combining the latest neuroscience with personalized luxury care, we aim to provide the environment where your brain’s healing capacity can finally be realized.